SEE MORE. TREAT MORE. CBCT IN GENERAL PRACTICE
It is clear that CBCT technology has brought tremendous advantages to dental diagnostics and treatment planning, especially in disciplines such as endodontics, implant planning and oral surgery. But what about 3D for General Dentistry?
“I’m not a specialist or doing complex cases. CBCT is more than I need.” – many GP’s disagree. One of these dentists is Dr. Daniel Butterman. He bought a 3D cone beam for one specific application, never expecting to utilise it across his entire practice. Today, it touches nearly everything and every patient he sees.
Versatile and powerful, crossing all types of dentistry
“I bought a 3D cone beam 10 years ago because I was getting into implants,” said Dr. Butterman, who has been practicing dentistry for 25 years. “I thought that was what I was buying it for. But it shocked me with all the other features and benefits. All of a sudden, it was like someone turned the light on because you can see things you couldn’t see before, from all angles. I was blown away.”
Today, he utilises his cone beam unit multiple times a day. And not just for implant patients, but for nearly every patient. It has replaced the 18 individual films his team used to capture in initial exams. The CBCT gives him more information up front, and also reduces the time his staff spends collecting those images. He uses it with restorative patients, in root canals, periodontics, extractions, orthodontics, and pretty much everything else. Dr. Butterman points to the abundance of data a cone beam delivers as the first and most powerful contributor to a practice’s ROI. “If I can’t see something, I can’t diagnose it, and I can’t treat it,” said Dr. Butterman. “A doctor will end up with more treatments just because he or she can see more things.”
Treatment Acceptance Skyrockets
A cone beam broadcasts hidden issues in the mouth and jaw so a doctor can see them and treat them. In addition, it also allows those problems to be shown to patients in real time so they can become partners in the diagnosis and advocates for their own oral health care. In a few seconds, patients can see things like bone density that may indicate the need for grafting, or a fracture in a hidden area of the tooth. This patient education helps them become more engaged in choosing options and more open to recommended solutions.
Cone beam images can be integrated with digital scans, so a crown can be planned in CAD/CAM software and imported into the 3D image. “Patients can see their jaw and final crown on the screen before we even make it,” noted Dr. Butterman. “It’s shocking to them. Case acceptance is night and day.” Cone beam images can also be downloaded into a DICOM file format and sent to other colleagues or other software used in the practice.
Predictable, Positive Outcomes
Another way a cone beam boosts ROI is in the speed and precision with which procedures can be done. If a doctor was doing an implant case without 3D imaging, he or she wouldn’t know for sure what they would find until they flapped the tissue. Or in the case of root canals, valuable time had to be spent surveying the canal and checking for extra canals. By knowing what’s waiting underneath before the procedure starts, a doctor can approach cases, particularly complex cases, with more confidence, according to Dr. Butterman.
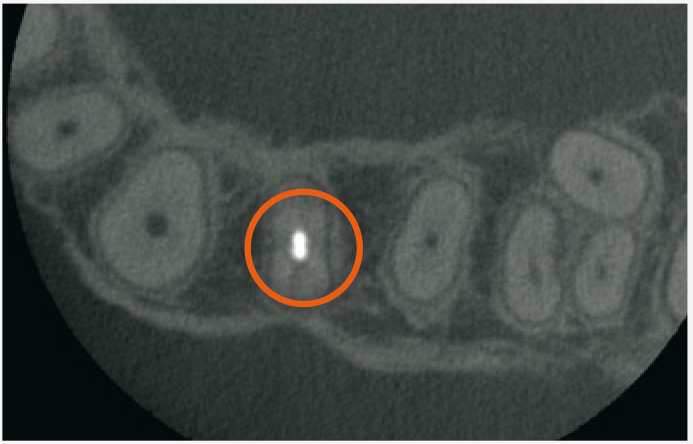
ROI isn’t just measured in what is done, but just as importantly, what doesn’t have to be redone or expanded into a longer appointment, or several. Dr. Butterman has had patients come in with existing root canals who admit the tooth has never felt right but they’ve just lived with it. Regular X-rays found nothing wrong, but then he takes a 3D image! “I can’t tell you how many root canals I’ve seen that have massive infections even though the patient is asymptomatic,” said the doctor. Patients are thrilled to finally have answers to causes of pain or discomfort that couldn’t be identified before, and the patient word-of-mouth travels far and fast…another intangible ROI.
Empowering Doctors to expand dentistry – More patients in, less referrals out
3D imaging also allows doctors to choose their cases with greater assurance. Dr. Butterman now takes on more complicated implant cases and extractions he believes he wouldn’t have done before, because he can see comprehensive detail. Conversely, he has chosen to refer cases that looked simple initially, but after seeing the 3D images, he realised were more challenging than expected. It gives doctors control of the type of dentistry they want to do. The ROI for a cone beam may not be as obvious as other technologies like same-day dentistry, but Dr. Butterman has experienced incredible production growth in the years he’s used his. The CBCT allows him to see oral health issues that he wouldn’t have seen any other way and solve them for patients. “It’s not immediately obvious, but the next thing you know, production will be up because you can see more and do more procedures,” explained Dr. Butterman.
Patient Safety and Health
The big contributors to a cone beam ROI are numerous:
- An increased number of cases that are identified due to precise images that capture obscure issues
- Efficiency of treating these cases when a doctor has complete detail about what to expect
- A higher rate of predictable outcomes when challenges can be planned for in advance
- Happy patients who receive and understand the diagnosis and buy in to your treatment
For Dr Butterman, all of those factors are key to his cone beam’s ROI, but there’s one factor that is even greater for him… a single patient experience in which the cone beam discovered a bony tumour. Dr Butterman referred the patient to his doctor, and the patient called back a few months later with news that the tumour had been malignant, and the scan had saved his life! “There is no greater ROI than that! We are in the business of solving problems,” concluded Dr Butterman. “Diagnosing is our job. If there’s a tool that makes our diagnoses more accurate, we owe it to ourselves—and our patients—to use it.”
SEE MORE. TREAT MORE. CBCT IN ENDODONTICS
Imagine walking down a dark pathway at night. You turn on a flashlight and suddenly you are alerted to things you couldn’t see before that could trip you up…tree roots, uneven ground, winding turns. That’s what a 3D cone beam imaging system does inside a patient’s mouth – it takes comprehensive, highly precise images that highlight the oral cavity and surrounding anatomy in ways that traditional 2D X-rays, the standard of care, isn’t able to do.
Cone Beam applications in Endodontics
LOCATING CANALS: Root canals are complex procedures, and one reason is the challenge of mapping the canals to be sure nothing is missed and every part of the infection is dealt with successfully. To have the best chance for a good outcome, all the canals should be seen and become a part of the treatment plan. 3D imaging helps Endodontists see how many canals there are, and where they are located. Doctors save a lot of time because they can see immediately if there are unusual anomalies, like a second mesiobuccal canal or missed lingual canals, or roots right on top of sinus cavities.
If there’s an anomaly, Endodontists know before beginning the procedure and can adjust their treatment plan accordingly. In fact, a study evaluated how treatment plans were affected when cone beam imaging data was added to cases vs. only traditional X-rays. It found in 62% of the cases, evaluators changed their treatment plans on the strength of the 3D images. This proves it significantly influences the direction and effectiveness of a patient’s treatment, when made available, presumably for the better.
DISCOVERING OTHER UNUSUAL PATHOLOGIES: 3D imaging can also help Endodontists see other conditions that are difficult, if not impossible, to see in intraoral X-rays: vertical root fracture, cracked teeth, or interior or exterior root reabsorption. A clinical assessment, which asks a lot of questions looking for red flags, is done alongside the 3D image.
DIAGNOSING PAIN: Most doctors have been frustrated when they are unable to find a reason for patient pain because X-rays and other clinical assessments haven’t located the source. Dr. Butterman uses his cone beam with almost every patient as he believes it gives him so much detailed information to discover the source of pain, helping solve problems that were previously mysteries.

SEE MORE. TREAT MORE. CBCT IN ORAL SURGERY
Before a single incision is made, many oral surgeons rely on a cone beam 3D imaging system to provide them with detail about the case. With a single rotation, 150-200 images are taken and then put together into a three-dimensional rendering with sophisticated, predictive software.
CBCT imaging is used most widely in oral surgery. It contributes valuable information applicable to many procedures done in the practice. With the insight it provides, oral surgeons can evaluate and preplan extractions, particularly of third molars; confirm measurements and proximity to other anatomical structures located close to the surgical site; and determine the quality and quantity of bone available for implant surgery.
In addition, 3D imaging allows oral surgeons to discover other pathology such as infections, tumours or cysts, and osteonecrosis. Implant dentistry and impacted tooth extraction are the two main uses for CBCT images.
Cone Beam helps evaluate site before surgery
Regardless of the procedure, the reason so many doctors rely on cone beam imaging is that it alerts them to potential concerns before they make an incision. They can identify areas of risk and prepare for them as well as share that information with patients. The result is a patient who is engaged with their care and a doctor who is certain of what he or she will find when the procedure begins. This leads to faster and more successful outcomes, which is particularly important when a patient is under anaesthesia.
Impacted teeth: Valuable for surgeries that involve third molars and supernumerary teeth, the cone beam, in a single pass, maps out important anatomical structures that are close to the impacted teeth, such as nerves and sinus cavities. 3D imaging does a better job than traditional X-rays in identifying root resorption in impacted canines and provides details on relationships with adjacent teeth so adjustments can be made to the surgical plan if needed.
Implant planning and placement: A growing number of doctors who place implants say they would not do them without using a cone beam. “In implant surgery there are a lot of issues and factors that you don’t know about until you flap tissue,” explained Dr Butterman. “It’s not predictable. Now I bring the image up and the patient gets to diagnose with me.” He notes that many times, patients come to him for a second opinion after an implant was recommended. Previously they only saw a 2D image, so they are confused and scared about treatment, particularly if the conversation involves bone grafting. He has found case acceptance increases when patients can see the 3D image. “If they need it, they know it,” said Dr. Butterman.
Doctors also gain valuable information about the quality and quantity of the bone and what size and length the implants should be. In complex cases with multiple implants, the 3D image is so precise, doctors can use it to fabricate surgical guides. The use of cone beam imaging further advances their dentistry and confidence in taking on complicated, multi-implant patients. The cone beam can also advise doctors and patients whether an implant should even be done. This knowledge can save a patient the time, expense, and frustration of a failed restoration. Discovering pathology: Just as valuable is the technology’s ability to see pathology not otherwise seen in exams or 2D X-rays. It’s not uncommon for an oral surgeon to recount cases where the cone beam identified tumours that turned out to be malignant.
SEE MORE. TREAT MORE. CBCT IN PERIODONTICS
Dental practices often purchase cone beam 3D imaging for a specific application. However, once doctors start using a cone beam, they discover it’s a jack-of-all-trades piece of equipment that’s more versatile and valuable than they thought. A cone beam reveals issues in the oral cavity that would otherwise go unnoticed, elevating the effectiveness of pre-treatment planning for more predictable outcomes.
In the field of periodontics, Periodontists diagnose and treat their patient’s teeth, supporting structure, and gums. The cone beam allows early diagnosis of issues around the tooth and its supporting bone and ligament structures that are not always seen by traditional 2D X-rays.
Being able to diagnose these problems early is important because the disease can progress with few obvious symptoms, damaging teeth and the surrounding bone. This is critical as advanced gum disease is linked to a higher incidence of diabetes, heart disease, and stroke, as well as loss of teeth.
Cone Beam more effective in detecting periodontal disease
The standard of care in diagnosing periodontal disease has been manual probing of pockets alongside 2D intraoral and panoramic X-rays. While those modalities still provide excellent clinical care, the 2D images do lose some detail by not capturing measurements of three-dimensional teeth. The only way to truly diagnose periodontal disease is through a detailed examination, so adding a more precise technology to catch signs of advancement is beneficial.
Cone Beam vital to implant dentistry
In addition to identifying advancing bone and structural damage from gum disease, the cone beam is nearly indispensable to Periodontists who have expanded their practice into implant dentistry. Dr. Peter Hunt, who operates a practice that focuses on implant dentistry, purchased a cone beam more than 15 years ago. He uses his unit multiple times every day as 3D imaging gives him the power to plan out every part of the implant procedure ahead of time. He plans the placement of the implant and mocks up the position of the restoration for patient viewing. In addition, 3D images give him the ability to display the bone region for an easy visual when he discusses bone grafting, if necessary.
“The cone beam gives me a much greater sense of comfort,” said Dr. Hunt. “In fact, in my opinion, doctors shouldn’t be placing an implant without one.” Dr. Butterman also uses the cone beam images to make choices about the complexity of cases he accepts, and to prepare for the scenarios involved in the procedure ahead of time. “When you do implant surgery, there are a lot of things you don’t know until you flap the tissue,” said Dr. Butterman. “I might have thought there was more bone support, or I wasn’t sure. Because of the cone beam, I can see that the implant can be done safely. It has let me confidently plan cases correctly.”
Are you thinking about setting up a new Dental Practice or renovating and redesigning your existing clinic? Check out Henry Schein’s Surgery Setup website for a range of resources and information to help you get sorted.
Be sure to keep an eye on Henry Schein’s Dental Education Hub for related events, courses, and information.